Orthopedic Initiatives
Alveolar bone and tooth constructs
In the United States, more than 70 million adults are potential candidates for dental implants. Approximately 5 million implants are placed each year, and results in one failure every four minutes. Implant failure is a major concern because re-implantations are increasingly difficult. Funded by the Department of Defense’s Armed Forces Institute of Regenerative Medicine II, this project aims to develop bioresorbable scaffolds that promote alveolar bone and tooth formation using autologous and/or allogeneic dental progenitor cell populations. The research team at the NJCBM is developing biphasic scaffolds that are able to regenerate tissue interfaces, such as the interface between bone and teeth. The biphasic scaffolds are fabricated as a single scaffold with two distinct polymer layers, one that supports the growth of one tissue type (e.g., bone), and the other that supports the growth of another tissue type (e.g., tooth). In this way, a scaffold with two well-integrated, yet distinct regions is obtained. The zone of integration is well defined and discrete. The long-term objectives of this project are to demonstrate safety and efficacy in small and large animal models. This work is a collaboration between Joachim Kohn’s laboratory at the NJCBM and Pamela Yelick’s laboratory at Tufts University.
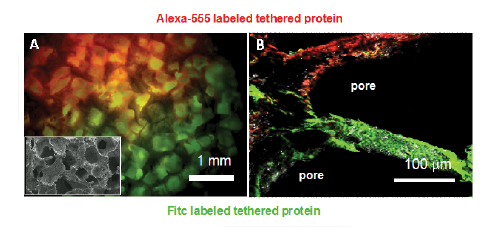
Spacial tethering of ligands within a single scaffold. (A-B) Confocal images of different fluorescent proteins tethered in a single scaffold forming a distinct interface, inset SEM in A shows pore structure.
Craniofacial and long bone defects
According to the American Association of Orthopaedic Surgeons, musculoskeletal conditions in the United States cost society more than $200 billion in medical care and lost productivity. Although orthopedic injuries in the civilian population are quite common, complex and extensive military combat-related orthopedic injuries (e.g., large gap defects) have increased the challenges of orthopedic treatment. Polymeric biomaterials have been successfully used in orthopedic applications, but are effective only as treatments for small bone defects (less than 3 cm). The team at the NJCBM aims to design, fabricate, and evaluate bioactive polymers to be used in polymer-based orthopedic devices that will speed healing of large bone defects (greater than 3 cm), while reducing both pain and medical costs. Funded by the Department of Defense’s Armed Forces Institute of Regenerative Medicine I and II, these projects aim to develop scaffolds for repairing large gaps in the cranium and long bones. These projects bring together leading academic and military research laboratories and clinicians, teams that combine world-class expertise in materials science, polymer chemistry, engineering, and biology. The research objectives of these projects are to demonstrate safety and efficacy in large animal bone defect models.
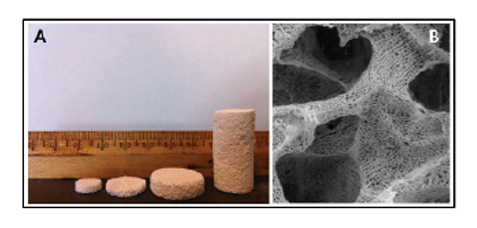
A) Photograph of tyrosine-derived polycarbonate bone regeneration scaffolds of varying dimensions fabricated by a combination of phase separation, freeze-drying, and salt-leaching. B) Scanning electron micrograph of tyrosine-derived polycarbonate bone regeneration scaffolds showing both macropores (for cell infiltration) and micropores (for diffusion and exchange of nutrients and waste).